
Identifying and targeting dysregulated pathways in autonomic neurons derived from CCHS patients
Dr. Gad Vatine, Ph.D., researcher at Ben-Gurion University of the Negev, Department o Physiology and Cell Biology, Faculty of Health Sciences and The Regenerative Medicine and Stem Cell (RMSC) Research Center
Dr. Avraham Ashkenazi, Ph.D., Department of Cell and Developmental Biology at Tel-Aviv University
Drs. Vatine and Ashkenazi are collaborating to investigate degradation pathways of misfolded PHOX2b.
Congenital Central Hypoventilation Syndrome (CCHS) is a rare and life-threatening condition presenting as central apneas during sleep to which there is currently no cure. CCHS is caused by mutations in PHOX2B, a key factor in the development and function of the autonomic nervous system (ANS).
The first steps towards finding a treatment for any disorder is to understand the disease-causing mechanisms. Mouse models for CCHS fail to either recapitulate disease-relevant symptoms or die shortly after birth, limiting our ability to study underlying mechanisms. Thus, generating human relevant models to study CCHS is of utmost importance.
This collaborative research is conducted by two researchers who complement each other. Dr. Gad Vatine from Ben-Gurion University is studying rare neurological disorders using patient-derived induced pluripotent stem cells (iPSCs). Dr. Avraham Ashkenazi from Tel Aviv University is investigating protein homeostasis mechanisms in trinucleotide repeat expansion diseases. Here, the two research teams will utilize patient-derived disease-in-a-dish models to uncover genes and pathways that are affected in CCHS. This model is based on iPSCs derived from CCHS patients and associated healthy family relatives that are differentiated into neurons of the ANS. The teams will combine cellular and electrophysiological studies to identify and target specific vulnerabilities in the human neurons. This work will lead to better understanding of the mechanisms and pathways affected in CCHS and will provide a platform to test potential modulators of the affected pathways, thereby helping to find potential therapeutic treatments.
$400,000/2 years
Role of Phox2b in mouse brain-stem autonomic neurons
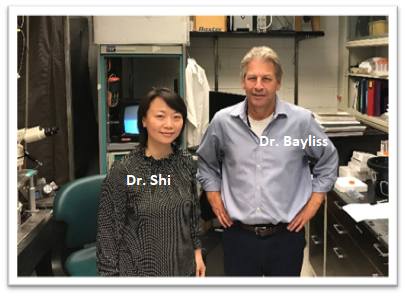
Dr. Yingtang Shi, M.D. Research Assistant and Professor, Department of Pharmacology, University of Virginia, Charlottesville, VA.
Dr. Douglas A. Bayliss, Ph.D. is the Joseph and Frances Larner Professor & Chair of Pharmacology at the University of Virginia, Charlottsville, VA.
Among the most salient signs in CCHS patients are the severe episodes of depressed breathing that manifest primarily during sleep, reflecting the absence of normal ventilatory and arousal responses to high CO2. In mouse genetic models of CCHS that incorporate a common CCHS-causing human mutation in the Phox2b gene, the primary deficit is that a group of CO2-sensing cells in the brainstem fail to develop. In this proposal, we utilize novel methods to determine the normal downstream targets for the cells missing in the CCHS mouse model, and to identify any specific genes expressed by those targets. Our hope is that this will provide new ideas that can be exploited in order to bypass the missing cells to help drive breathing and arousal during sleep.
approaches, supported by the CCHS Network, their group provided the first insights into the unique molecular genetics of a specific respiratory chemoreceptor, the retrotrapezoid nucleus, which contributes to breathing and waking reflexes activated by hypoventilation. In the proposed work, the team will take advantage of these approaches to knockdown Phox2b expression in multiple brainstem autonomic and respiratory chemoreceptor neurons to determine effects on cell viability, transcriptomic profiles, and regulation of breathing and arousal. Distributed disruption of Phox2b expression in these cell groups may underlie the dysregulated breathing, dysautonomia and dysfunctional arousal that characterize CCHS. This study will reveal the molecular and cellular mechanisms of CCHS pathogenesis that ignites hope for rational gene/cell therapies for CCHS.
$75,000/1 year
The lncRNA PHOX2B-AS1 in the pathogenesis and as potential drug target in Congenital Central Hypoventilation Syndrome (CCHS)
Dr. Jorge Gallego, Ph.D, Inserm research director at Robert Debré Hospital (Université de Paris)
Dr. Fornasari and his team propose to study the role of a recently identified regulatory non-coding RNA (PHOX2B-AS1) in CCHS pathogenesis and to evaluate its potentiality as a therapeutic target. In fact, an emerging concept in molecular genetics and biology is that regulatory RNAs play key roles in regulating gene expression and that their dysregulation may be involved in a large number of diseases and could be therapeutic targets. Preliminary data show that PHOX2B-AS1 promotes the production of PHOX2B protein, thus suggesting that manipulating its expression may reduce or normalize gene expression in CCHS by reducing mutant proteins toxic effects. In the proposed work, the team will take advantage of small oligonucleotides called “gapmers” to decrease the regulatory RNA so that PHOX2B mRNA translation can be reduced. Due to the unavailability of viable CCHS mice models to study the function of PHOX2B-AS1, the research group has recently generated induced pluripotent stem cells (iPSCs) from two CCHS patients to be differentiated into autonomic sympathetic neurons. In the proposed research, the team will combine molecular and cellular approaches to manipulate PHOX2B-AS1 RNA levels during the differentiation process of healthy and disease-derived iPSCs, to explore the possibility of PHOX2B-AS1 therapeutic targeting to reduce the toxic effect of mutant protein.
$75,000/1 year
 BY
BY